Abmp soap notes plantillas, contratos y formularios.
What is the format for SOAP notes?
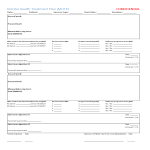
SOAP is an acronym for Subjective, Objective Assessment and Plan, which is a method of documentation common in the health and healthcare industry. SOAP Notes are therefore often considered a clinical document used in many healthcare organizations. This resource discusses the audience and purpose of the SOAP specification, suggested content for each section, and examples of appropriate and inappropriate language.
SOAP Notes are a common way for healthcare and other teams to organize the information they need to share with each other as they collaborate or pick up where others left off. SOAP annotations should be clear, well-written, and easy to understand so your team can find the information they need.
A good SOAP description should help healthcare professionals better document, retrieve, and apply detailed information about a specific case, thereby improving the quality of patient care.