HTML Preview Psychotherapy Tracking Form page number 1.
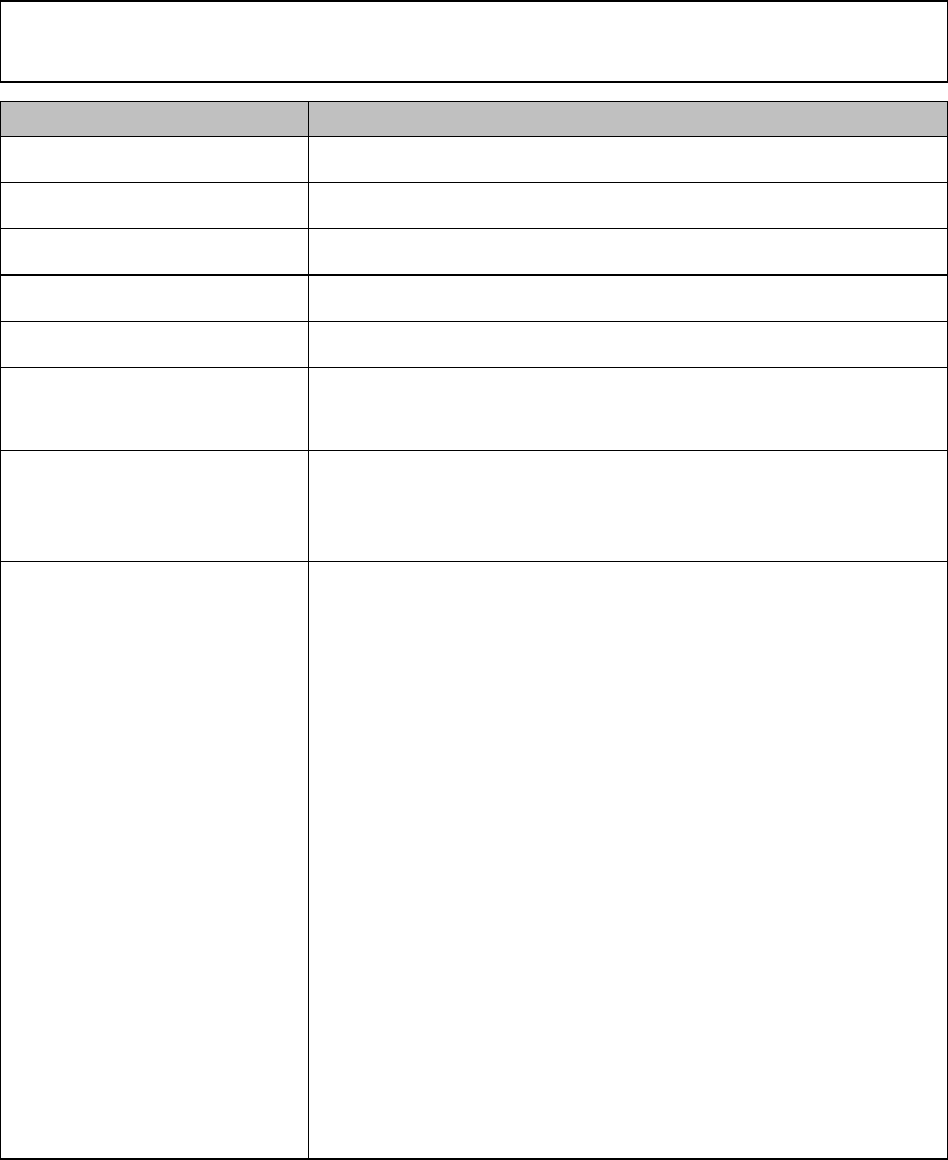
Psychotherapy Progress Note
Use this note to document individual, family or couples psychotherapy sessions and person’s response
to the intervention during a specific contact.
Data Field
Person’s Name
Record the first name, last name, and middle initial of the person. Order of name is at
agency discretion.
Record Number
Record your agency’s established identification number for the person.
Person’s DOB
Record the person’s date of birth.
Organization Name:
Record the organization for whom you are delivering the service.
Modality
Check appropriate box to indicate the type of session: individual, family or couple.
List Name(s) of Person(s)
Present
Check appropriate box to indicate whether the person is Present, is a No
Show/Cancelled or the Provider Cancelled. For cancellations, complete Explanation as
needed. Check appropriate box to indicate if others are present, list name(s) and
relationship(s) to person.
Person’s Report of
Progress Towards
Goals/Objectives Since
Last Session
Document person’s self-report of progress towards goals since last session including
other sources of information, such as family, case manager, etc..
New Issue(s) Presented
Today
There are four options available for staff using this section of the progress note:
1. If person does not report/present any new issues, mark “None Reported”
and proceed to planned intervention/goals.
2. If person reports a new issue that was resolved during the session check
the “New Issue resolved, no CA Update required” box. Briefly document
the new issue, identify the interventions used in the Therapeutic
Interventions Section and indicate the resolution in the Response Section
of the progress note.
Example: Person described being involved in a minor car accident today.
Person was not hurt but expressed concern regarding expense of car
repair. Person felt more relieved after identifying ways to cover expense
over the next two weeks.
3. If person presents an issue that has been previously assessed and for
which Goals/Objectives and services have been ordered, then the
information may be briefly documented as an indicator of the progress or
lack of progress achieved.
4. If person presents any new issue(s) that represent a therapeutic need that
is not already being addressed in the IAP, check box indicating a “CA
Update Required” and record notation that new issue has been recorded
on a Comprehensive Assessment Update of the same Date and write
detailed narrative on the appropriate CA Update as instructed in this
manual. Also, the newly assessed therapeutic information may require a
new goal, objective, therapeutic intervention or service that will require
further use of the IAP Review/Revision form.
Example: Person reported for the first time that she was a victim of
abuse/neglect at the age of twelve as recorded on the
Comprehensive Assessment Update of this date.