HTML Preview Patient Note page number 1.
Copyright ©2014-16 by the National Board of Medical Examiners (NBME
) and the Educational Commission for Foreign Medical Graduates
(ECFMG
).
CLINICAL SKILLS EVALUATION
PATIENT NOTE
HISTORY: Describe the history you just obtained from this patient. Include only information (pertinent positives and negatives)
relevant to this patient’s problem(s).
Ms. Bingham is a 24 yo woman who complains of worsening sore throat since yesterday
morning. She has never had a similar problem in the past. She has no difficulty
swallowing, but notes that swallowing makes the pain worse. Nothing makes it better.
There is no SOB or sensation of choking or dysphagia. She has fatigue and has had some
anorexia since the symptoms began. She has had some subjective fevers at home but has not
taken her temperature. She has had no cough or rhinorrhea. There are no sick contacts at
home or at work. She denies seasonal allergies and post-nasal drip.
ROS: No chest pain, cough, wheezing, abdominal pain, N/V, headache
PMHx: none
Meds: none; Allergies: none
PSHx: none
FHx: father with HTN
SHx: married with 2 children, No ETOH or drugs, monogamous with husband
PHYSICAL EXAMINATION: Describe any positive and negative findings relevant to this patient’s problem(s). Be careful to include only
those parts of examination you performed in this encounter.
She is in no acute distress, throat clear, abdomen soft, nontender and without
distension. There is no notable splenic or hepatic enlargement or tenderness.
DATA INTERPRETATION: Based on what you have learned from the history and physical examination, list up to 3 diagnoses that might
explain this patient’s complaint(s). List your diagnoses from most to least likely. For some cases, fewer than 3 diagnoses will be
appropriate. Then, enter the positive or negative findings from the history and the physical examination (if present) that support
each diagnosis. Lastly, list initial diagnostic studies (if any) you would order for each listed diagnosis (e.g. restricted physical exam
maneuvers, laboratory tests, imaging, ECG, etc.).
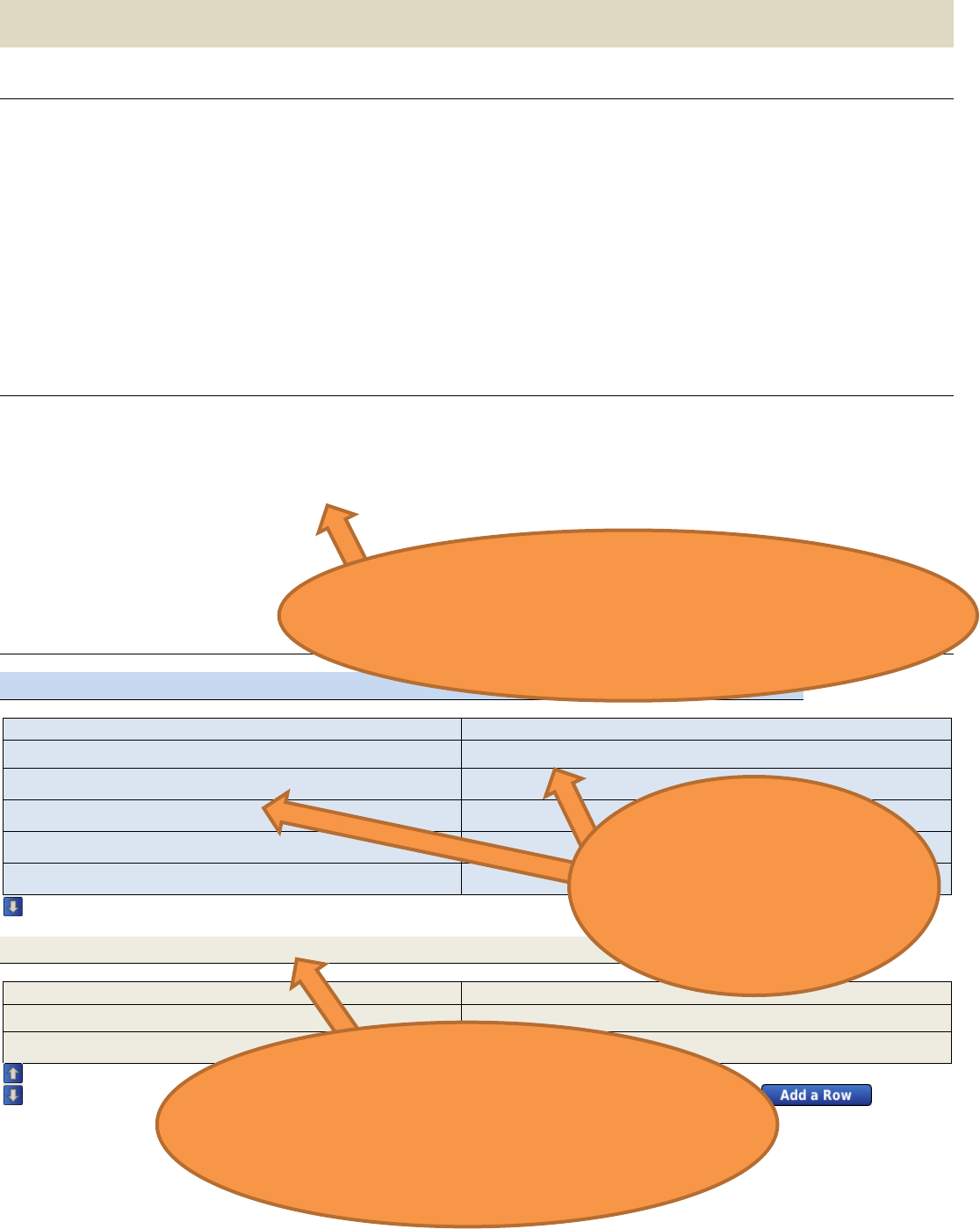
DIAGNOSIS #1: Viral Pharyngitis
HISTORY FINDING(S)
PHYSICAL EXAM FINDING(S)
Sore throat
Tender submandibular lymph nodes
Subjective fever
Fatigue
Anorexia
Pain with swallowing
DIAGNOSIS #2: Bacterial Pharyngitis/Retropharyngeal Abscess
HISTORY FINDING(S)
PHYSICAL EXAM FINDING(S)
Appropriate supporting
information is drawn from
the history and PE section
above and used to support a
likely diagnosis
Including a diagnosis without supporting
information would result in a lower score even if
the diagnosis is likely. Including two diagnoses on
the same line would result in a lower score.
The physical exam includes a cursory examination of the
throat. A higher level of detail such as specific mention of
erythema or exudate, and evaluation for regional
lymphadenopathy would result in a higher score.