Treatment Plan Template
Save, fill-In The Blanks, Print, Done!
Download Treatment Plan Template
Today: USD 4.99
Download It Now

Available premium file formats:
Microsoft Word (.docx)- This Document Has Been Certified by a Professional
- 100% customizable
- This is a digital download (66.13 kB)
- Language: English
- You will receive a link to download the file as soon as your payment goes through.
- We recommend downloading this file onto your computer.
How do you write a treatment plan? What does a treatment plan consist of? Are you in need of a professional Mental Health Treatment Plan?
A mental health treatment plan is a document that contains and outlines the details of a client's current mental health issues and outlines the goals, targets, and strategies that will assist the client in overcoming mental health issues. To obtain the information needed to complete a treatment plan, a health worker must interview the client. The information gathered during the interview is used to write the complete treatment plan.
Steps to proceed when setting up plan:
A: Health Assessment
- Gather information. A psychological evaluation is a fact-gathering session in which a mental health worker (counselor, therapist, social worker, psychologist, or psychiatrist) interviews a client about current psychological problems, past mental health issues, family history, and current and past social problems with work, school and relationships.
- Follow the sections of the evaluation. Most health facilities provide the mental health worker with a template or form to complete during the interview.
- Note behavioral observations. The counselor will conduct a mini-mental status exam which involves observing the client's physical appearance and his or her interactions.
- Make a diagnosis. The diagnosis is the main focus. Sometimes a client will have multiple diagnoses such as both Major Depressive Disorder and Alcohol Use. Diagnoses must be complete before a treatment plan can be completed.
- Determine reachable goals
- Once you have completed the initial assessment and made a diagnosis, you will want to think about what interventions and goals you might want to create for treatment.
- Think of interventions. The interventions are the meat of change in therapy. Your therapeutic interventions are what will ultimately evoke change in your client.
- Discuss goals with the client. After the initial assessment is conducted, the therapist and client will collaborate to create appropriate goals for treatment.
- Make concrete goals for treatment. The goals are also what make up a large component of the treatment plan. Use the SMART method
- Record the treatment plan's components. The treatment plan will consist of the goals that the counselor and therapist have decided on. Many facilities have a treatment plan template or form that the counselor will fill out. Part of the form may require that the counselor checkboxes that describe the client's symptoms.
- Write down the goals. Your goals need to be clearly defined. Remember the SMART goals plan and make each goal specific, measurable, achievable, realistic, and time-limited.
- Express specific interventions you will use. The counselor will include treatment strategies the client has agreed to.
- Sign the treatment plan. Both the client and the counselor sign the treatment plan to show that there is an agreement on what to focus on in treatment.
- Review and improve as needed. No plan is perfect. You will be expected to complete goals and make new ones as the client progresses in treatment. The treatment plan should include dates in the future that the client and counselor will review the progress the client is making. Decisions to continue the current treatment plan or to make changes will be made at that time.
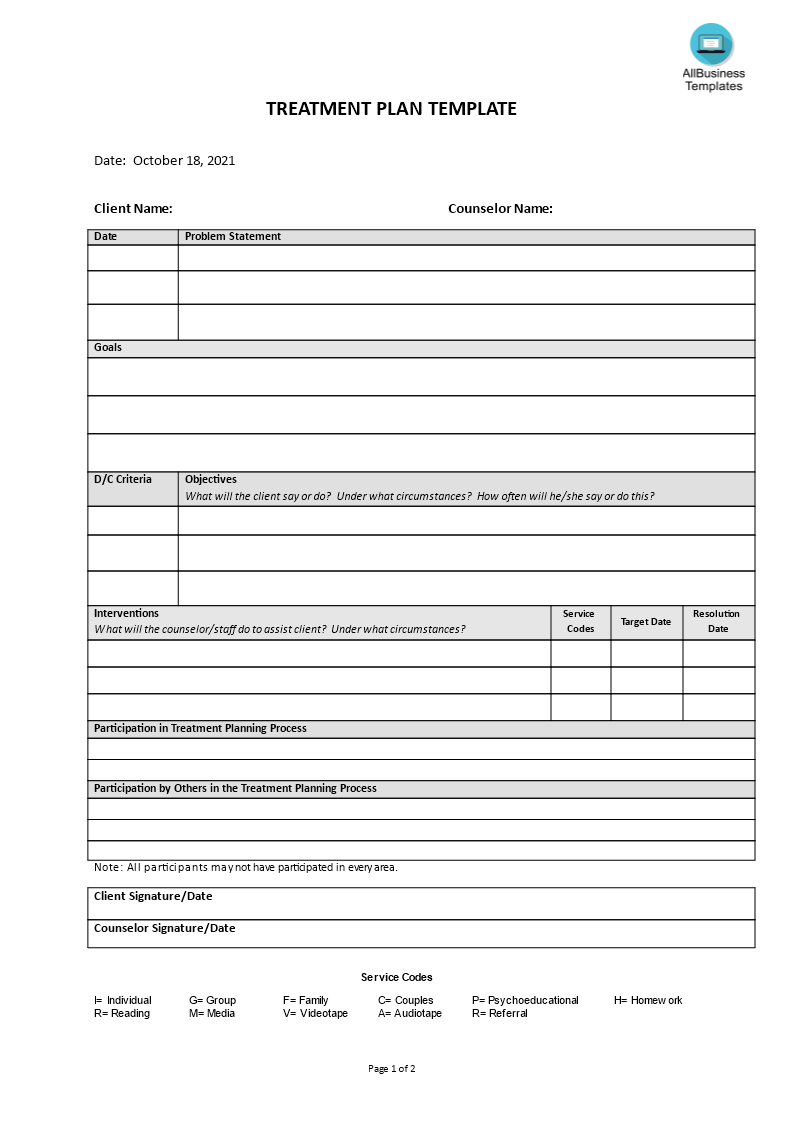
Treatment Plan:
- Client Name
- Counselor Name
- Date
- Problem Statement
- Goals
- D/C Criteria Objectives
- How often will he/she say or do this?
- Interventions
- Service Codes
- Target Date Resolution
- Participation in Treatment Planning Process
- Participation by Others in the Treatment Planning Process
- Note: All participants may not have participated in every area.
- Service Codes:
- I= Individual
- G= Group
- F= Family
- C= Couples
- P= Psychoeducational
- H= Homework
- R= Reading
- M= Media
- V= Videotape
- A= Audiotape
- R= Referral
Try out our online Free and Premium Professional templates, forms, and contracts today. Save, fill-In the blanks, print …and done!
Download this Health Treatment Plan template now!
DISCLAIMER
Nothing on this site shall be considered legal advice and no attorney-client relationship is established.
Leave a Reply. If you have any questions or remarks, feel free to post them below.
Related templates
Latest templates
Latest topics
- Formal Complaint Letter of Harrasment
How do I write a formal complaint about harassment? Check out these formal complaint letter of harrasment templates here! - Google Sheets Templates
How to work with Google Sheets templates? Where to download useful Google Sheets templates? Check out our samples here. - Letter Format
How to format a letter? Here is a brief overview of common letter formats and templates in USA and UK and get inspirited immediately! - IT Security Standards Kit
What are IT Security Standards? Check out our collection of this newly updated IT Security Kit Standard templates, including policies, controls, processes, checklists, procedures and other documents. - Excel Templates
Where do I find templates for Excel? How do I create a template in Excel? Check these editable and printable Excel Templates and download them directly!
cheese